Expert diagnosis and treatment in Hampshire
High cholesterol, medically termed hyperlipidaemia, occurs when you have elevated levels of cholesterol or other fats (lipids) in your bloodstream. Cholesterol exists in several forms: LDL cholesterol (often called “bad” cholesterol) contributes to plaque buildup in arteries, whilst HDL cholesterol (“good” cholesterol) helps remove cholesterol from your bloodstream. Triglycerides are another type of blood fat that can increase cardiovascular risk when elevated.
Cholesterol levels are influenced by both genetic and lifestyle factors. Some individuals have familial hypercholesterolaemia, an inherited condition causing very high cholesterol from birth. For most people, high cholesterol develops through a combination of dietary factors (particularly saturated fat intake), lack of physical activity, being overweight, smoking, and increasing age. Certain medical conditions including diabetes, hypothyroidism, and kidney disease can also elevate cholesterol levels. Understanding your specific risk factors allows for targeted treatment approaches.
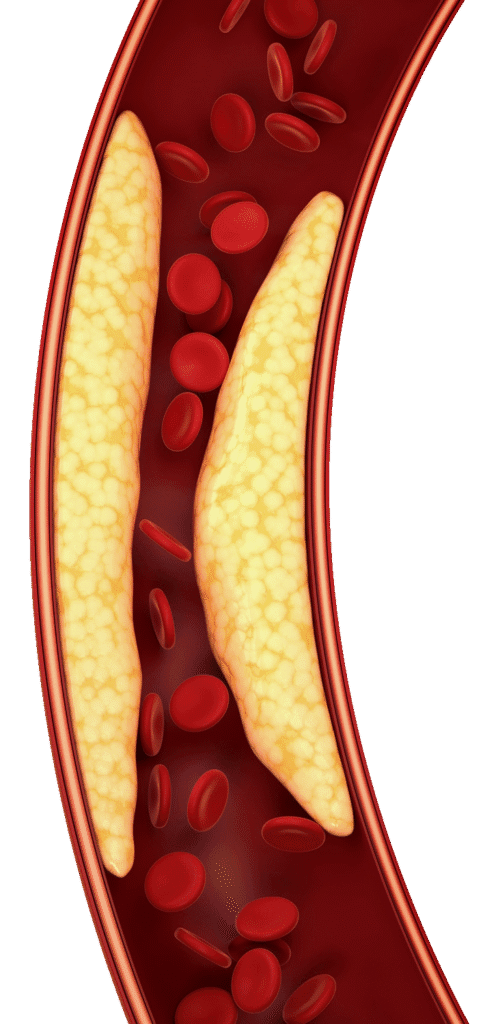
Elevated cholesterol represents a major risk factor for cardiovascular disease. When LDL cholesterol levels remain high, cholesterol deposits accumulate in artery walls, forming plaques that narrow and stiffen arteries—a process called atherosclerosis. This increases your risk of coronary artery disease, heart attack, and stroke. The concerning aspect of high cholesterol is that it typically causes no symptoms until significant arterial disease has developed, making screening and early treatment essential for preventing cardiovascular complications.
High cholesterol typically causes no symptoms, but certain signs and risk factors indicate you should have your cholesterol checked:
Close relatives with early heart disease or high cholesterol, especially familial hypercholesterolaemia.
Previous heart attack, angina, stroke, or peripheral arterial disease requiring cholesterol management.
Diabetes, high blood pressure, smoking, or being significantly overweight increase your risk.
Men over 40 and women over 50, or post-menopausal, have increased cardiovascular risk.
Rarely, very high cholesterol causes xanthomas (cholesterol deposits under skin) or corneal arcus (cholesterol around the pupil).
Regular screening recommended for adults, especially with multiple cardiovascular risk factors.
Cholesterol assessment begins with a comprehensive cardiovascular risk evaluation. A detailed consultation explores your family history, lifestyle factors, existing medical conditions, and any medications you’re taking. Understanding these elements helps identify your specific cholesterol concerns and determines whether high cholesterol represents an isolated problem or part of a broader cardiovascular risk profile. This personalised assessment forms the foundation for tailored treatment recommendations.
A lipid profile blood test measures your total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. Ideally performed after fasting, this test provides crucial information about your cardiovascular risk. For some patients, advanced lipid testing may be recommended to assess specific cholesterol particles and lipoproteins. When familial hypercholesterolaemia is suspected, genetic testing can confirm the diagnosis. These investigations allow precise characterisation of your lipid disorder and guide treatment intensity.
Your overall cardiovascular risk is calculated using validated scoring systems that consider your cholesterol levels alongside other risk factors including age, blood pressure, diabetes status, and smoking history. When appropriate, additional cardiac investigations such as coronary calcium scoring with cardiac CT, echocardiography, or carotid ultrasound may be performed to assess for existing arterial disease. This comprehensive evaluation determines your treatment targets and helps monitor the effectiveness of cholesterol-lowering interventions over time.
High cholesterol management requires a personalised approach combining lifestyle modifications with medication when necessary. Treatment intensity depends on your overall cardiovascular risk, cholesterol levels, and individual circumstances. Dr Cassar works with you to develop an effective, evidence-based treatment plan targeting optimal cholesterol control and cardiovascular risk reduction.
Treatment begins with comprehensive cardiovascular risk stratification, determining whether you’re at low, moderate, high, or very high risk of future cardiovascular events. This assessment considers your cholesterol levels, age, blood pressure, diabetes status, smoking history, family history, and any existing cardiovascular disease. Your risk category determines treatment targets—those at higher risk require more aggressive cholesterol lowering.. Regular risk reassessment ensures treatment remains appropriately intensive as circumstances change.
Dietary changes form the foundation of cholesterol management. Reducing saturated fat intake by limiting red meat, full-fat dairy, and processed foods whilst increasing consumption of vegetables, fruits, whole grains, and oily fish can significantly improve lipid profiles. Regular physical activity—aiming for 150 minutes of moderate exercise weekly—helps raise HDL cholesterol and lower triglycerides. Achieving a healthy weight, stopping smoking, and moderating alcohol intake all contribute to better cholesterol levels. For some individuals with mild cholesterol elevation and low cardiovascular risk, lifestyle changes alone may be sufficient. Practical dietary advice and exercise recommendations are provided to support sustainable lifestyle improvements.
Statins represent the cornerstone of cholesterol-lowering medication, proven to significantly reduce cardiovascular events and mortality. These medications work by inhibiting cholesterol production in the liver, typically lowering LDL cholesterol by 30-50%. Modern statins are generally well-tolerated with an excellent safety profile. Treatment usually begins with moderate-intensity therapy, with dose adjustment based on cholesterol response and tolerability. Whilst muscle discomfort affects a small percentage of patients, most people tolerate statins without problems. Regular monitoring with blood tests assesses treatment effectiveness and safety. The proven cardiovascular benefits of statins far outweigh risks for most patients requiring cholesterol-lowering medication. For patients unable to tolerate statins, those not achieving target cholesterol levels despite maximum statin therapy, or individuals with familial hypercholesterolaemia, additional effective treatments can be used.
Successful cholesterol management requires regular follow-up to monitor treatment effectiveness, assess tolerability, and adjust therapy as needed. Repeat lipid profiles typically occur 6-12 weeks after starting treatment, then annually once stable target levels are achieved. Monitoring also includes checking for medication side effects through blood tests assessing liver and muscle function. Your cardiovascular risk profile is periodically reassessed as you age or if other risk factors develop. Treatment is optimised to maintain cholesterol at target levels whilst minimising medication burden. Long-term cholesterol control significantly reduces your risk of heart attack and stroke, making sustained treatment adherence essential for cardiovascular protection.
Cholesterol is a waxy, fat-like substance that your liver produces. Your body needs cholesterol to make cell membranes, hormones, and vitamin D. The problem isn’t cholesterol itself—it’s having too much of the wrong type. There are two main types: LDL (“bad” cholesterol) which builds up in your artery walls, and HDL (“good” cholesterol) which helps remove cholesterol from your bloodstream. High LDL cholesterol increases your risk of heart attacks and strokes because it forms plaques that narrow and harden your arteries over time.
Think of LDL (low-density lipoprotein) as delivery trucks carrying cholesterol from your liver to your arteries—too many trucks mean cholesterol gets deposited in artery walls, causing blockages. HDL (high-density lipoprotein) acts like rubbish collectors, picking up excess cholesterol and taking it back to your liver for disposal. You want your LDL as low as possible (less cholesterol being delivered to arteries) and your HDL reasonably high (more cholesterol being removed). That’s why we call LDL “bad” and HDL “good”—though really, you need both to be balanced properly.
You can’t feel high cholesterol—it causes no symptoms until serious problems develop, which is why it’s often called a “silent” condition. The only way to know is through a simple blood test called a lipid profile, which measures your total cholesterol, LDL, HDL, and triglycerides (another type of blood fat). Adults should have cholesterol checked at least once between ages 20-30, then regularly thereafter—more frequently if you have risk factors like family history, high blood pressure, diabetes, or being overweight.
For most people, high cholesterol develops from a combination of diet (particularly foods high in saturated fats like red meat, full-fat dairy, and processed foods), lack of exercise, being overweight, and smoking. Your genes also play a role—some people inherit familial hypercholesterolaemia, causing very high cholesterol from birth regardless of lifestyle. Age matters too—cholesterol naturally tends to rise as we get older. Certain conditions like diabetes, underactive thyroid, and kidney disease can also raise cholesterol levels.
This isn’t a simple answer because target levels depend on your individual cardiovascular risk. Generally, total cholesterol should be below 5mmol/L and LDL below 3mmol/L for healthy people. But if you have diabetes, previous heart attack, or multiple risk factors, your targets will be stricter—sometimes LDL below 1.4 or even 1.1mmol/L. HDL should ideally be above 1.0mmol/L for men and 1.2mmol/L for women. Your doctor calculates your personal risk score considering all your risk factors, then recommends specific targets for you. It’s not one-size-fits-all.
For some people, yes. Lifestyle changes can lower LDL cholesterol by 5-15%, sometimes more with very strict diets. If your cholesterol is only mildly elevated and your overall cardiovascular risk is low, diet and exercise alone might be enough. The most effective changes include cutting saturated fats (red meat, butter, full-fat dairy), increasing fibre (oats, beans, vegetables, fruits), eating more unsaturated fats (nuts, olive oil, oily fish), losing excess weight, exercising regularly, and stopping smoking. However, if your cholesterol is very high or you have other risk factors, medication will likely be necessary alongside lifestyle changes to adequately protect your heart.
Focus on foods rich in soluble fibre—oats, barley, beans, lentils, apples, and citrus fruits—which help remove cholesterol from your body. Eat plenty of vegetables and include nuts, especially almonds and walnuts. Choose oily fish like salmon, mackerel, and sardines twice weekly for omega-3 fats. Use olive oil or rapeseed oil instead of butter. Foods fortified with plant sterols (certain margarines, yoghurts, and milk drinks) can lower LDL by 7-10%. Basically, eat more plants, choose healthy fats, and include oily fish—it’s the Mediterranean diet approach.
Limit foods high in saturated fats: red meat, processed meats (sausages, bacon), full-fat dairy products (butter, cream, cheese), and processed snack foods. Avoid trans fats completely—check labels for “partially hydrogenated oils” though these are increasingly rare in UK foods. Cut back on baked goods, pastries, and fried takeaway foods. You don’t have to eliminate these entirely, but reduce portion sizes and frequency. Swap full-fat milk for semi-skimmed, choose leaner meats, and grill rather than fry. Small changes add up.
Yes, absolutely. Regular exercise raises HDL (“good” cholesterol), lowers triglycerides, and can modestly reduce LDL. Aim for at least 150 minutes of moderate activity weekly—brisk walking, cycling, swimming, or any activity that gets your heart pumping. Exercise also helps with weight management, blood pressure, and overall cardiovascular health. You don’t need to run marathons—even regular walking makes a difference. The key is consistency. Combined with healthy eating, exercise significantly improves your cholesterol profile and reduces heart disease risk.
This depends on your overall cardiovascular risk, not just your cholesterol number. If you’ve had a heart attack or stroke, you definitely need statins—they dramatically reduce risk of another event. If you have diabetes, very high cholesterol, or multiple risk factors, statins are usually recommended because the benefits far outweigh any risks. If your cholesterol is only mildly elevated with no other risk factors, lifestyle changes might be tried first. Your doctor uses risk calculators considering your age, blood pressure, smoking status, and family history to determine if statins are necessary for you specifically.
Statins are among the most studied, safest, and most effective medications available. They’ve been used for over 30 years by millions of people. Most people tolerate them without any problems. About 5-10% experience muscle aches, which usually resolve by switching to a different statin or adjusting the dose. Serious side effects are very rare. The proven benefits—reducing heart attacks, strokes, and deaths by 30-40%—far outweigh the small risk of side effects for most people who need them. If you experience side effects, discuss them with your doctor rather than just stopping—there are often solutions.
Usually long-term, often lifelong. High cholesterol is typically a chronic condition—when you stop medication, cholesterol levels rise again within weeks. Think of it like glasses for poor eyesight: you need to keep wearing them to see clearly. The medication protects your heart continuously, reducing your risk of heart attack and stroke. This doesn’t mean you can’t make lifestyle changes—combining medication with healthy habits gives you the best possible protection. Some people with only modestly elevated cholesterol who make dramatic lifestyle changes might eventually reduce or stop medication under close medical supervision, but this is uncommon.
Several other medications can lower cholesterol if you can’t tolerate statins or if statins alone aren’t enough. These include ezetimibe (which blocks cholesterol absorption), PCSK9 inhibitors (very powerful injections used for very high cholesterol or familial hypercholesterolaemia), bempedoic acid, and fibrates (mainly for high triglycerides). Some people ask about supplements like red yeast rice or plant sterols—these can help modestly but aren’t substitutes for prescription medications when those are needed. Your cardiologist can advise on the best options for your situation.
You should see a cardiologist if your cholesterol is very high (LDL above 5mmol/L), if you have familial hypercholesterolaemia (very high cholesterol running in your family), if you can’t tolerate statins, if your cholesterol isn’t controlled despite maximum treatment, or if you have cholesterol alongside other cardiac risk factors or established heart disease. Specialist assessment ensures accurate diagnosis, access to advanced treatments, and personalised management. Early specialist input is particularly important for familial hypercholesterolaemia as close relatives may also need screening and treatment.
Dr Cassar provides comprehensive cholesterol assessment at his Hampshire clinics, including detailed cardiovascular risk evaluation and lipid testing. He’ll review your family history, lifestyle, and other risk factors to calculate your personalised risk score and determine appropriate cholesterol targets. Using advanced cardiac imaging when needed, he can assess for existing arterial disease. He’ll create a tailored treatment plan combining practical lifestyle advice with appropriate medication, monitoring your response and adjusting treatment to achieve optimal cholesterol control whilst minimising side effects. If you have complex lipid disorders or familial hypercholesterolaemia, he can coordinate specialist lipid clinic referrals.
Dr Cassar will discuss your medical history, family history of heart disease or high cholesterol, current diet and exercise habits, and any symptoms or concerns. He’ll examine you and arrange blood tests for a full lipid profile (and other relevant tests like diabetes screening). He’ll calculate your cardiovascular risk score to determine your cholesterol targets. Based on this comprehensive assessment, you’ll discuss whether lifestyle changes alone are sufficient or if medication is recommended. You’ll receive practical dietary advice and a clear treatment plan. Follow-up appointments monitor your cholesterol response and ensure treatment is working effectively.
Contact Dr Cassar’s practice directly to arrange your consultation. He sees patients at Candover Clinic in Basingstoke and in Winchester. Whether you have newly diagnosed high cholesterol, aren’t achieving target levels despite treatment, have concerning family history, or want specialist cardiovascular risk assessment, early consultation ensures optimal management and protection of your heart health.
There are excellent resources to support you in managing high cholesterol: